Why Medicare Needs to Incentivize More Access to Home Health
Why Medicare Needs to Incentivize More Access to Home Health
Written by Julie B. Kennedy, CEO & Co-Founder, RubyWell
- A new report published in partnership with RubyWellTM shows that expanded usage of home health care services could save Medicare $13-17 billion per year.
- Increased home health aide support appears to contribute to lower overall expenditures and improved health outcomes for Medicare.
- CMS has proposed a 6.4% payment cut to Home Health services, which would reduce access to home health, driving up cost of care up via increased ER, in-patient, and SNF usage.
- Now is the time to advocate for rules that incentivize more access to home health care, not cut reimbursement for these services.
Medicare spends about $15.7 billion annually on home health care, according to The Medicare Payment Advisory Commission (MedPAC). That may sound like a lot of money. Because it is. But it amounts to less than 2% of Medicare’s total projected 2025 budget of $942 billion.
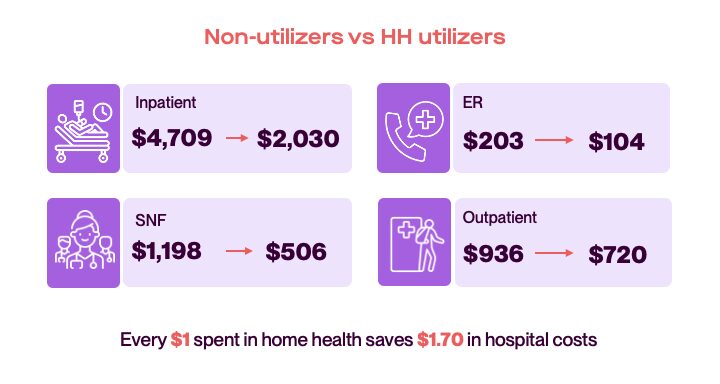
Meanwhile, medically necessary Home Health Care, if delivered to all those who meet criteria, could save Medicare $13-17 billion per year. How? By reducing ER visits, in-patient care, and skilled nursing facility (SNF) care. So for Medicare, home health care can effectively pay for itself.
CMS has proposed a multitude of home health care policy changes for calendar year 2026. Among them is a 6.4% payment cut to Home Health services. This should be deeply concerning to everyone. Cutting payment rates will push many home health providers out of a market where real margins are already razor thin, resulting in even fewer patients accessing care.
New report shows home health’s value
An analysis of 2023 Medicare Fee-for-Service claims from the Limited Data Set shows that Medicare beneficiaries using home health services cost Medicare 42% less than beneficiaries with similar health conditions who don’t use home health services. That savings equates to $3,600 per member per month (PMPM).
The full, downloadable report, “Evaluation of Home Health Expenditures in a Medicare-Eligible Population,” was prepared by a third party actuarial firm in partnership with RubyWell.
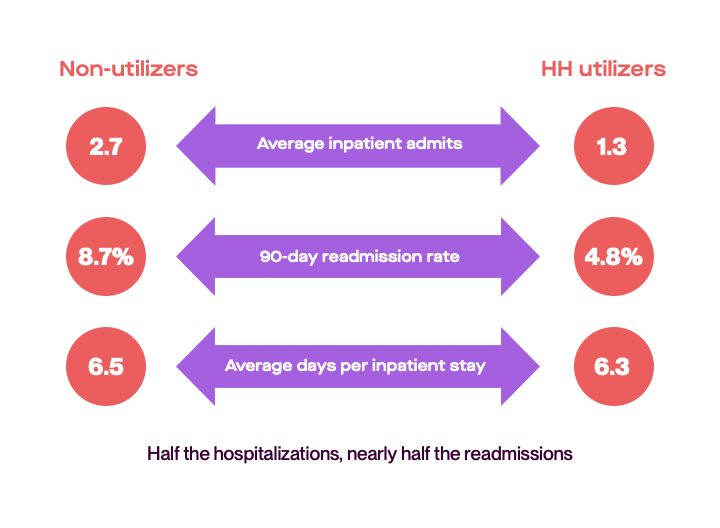
As part of the analysis, healthcare costs for home health users and non-users were compared. The cost savings and patient outcomes, when normalized by patient risk score, are irrefutable.
Home health delivers better outcomes & lower costs
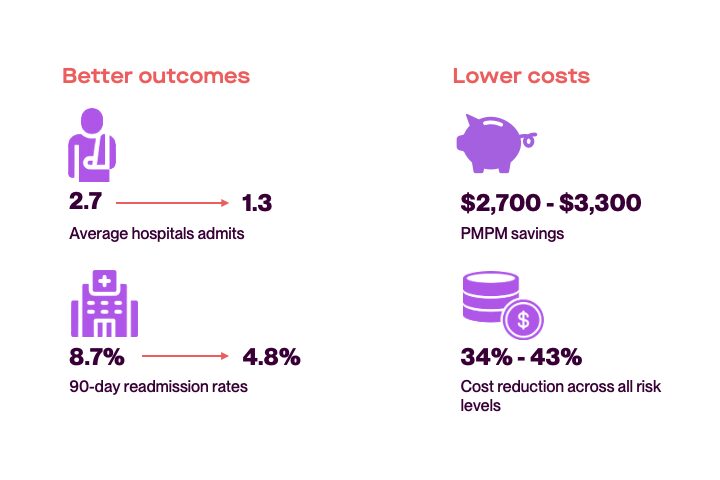
Home health lowers system usage
Home health keeps patients out of the hospital longer
The gist of these findings isn’t surprising to those working in the home health space. But having data-backed evidence of the true value of home health is invaluable in advocacy efforts to ensure accessibility to this cost saving care model.
RubyWell submitted a comment, including a copy of our report, to the CMS CY 2026 Home Health Prospective Payment System proposed rule, along with over 900,000 other concerned citizens.
While the comment period on the proposed rule has closed, now is the time to dial up advocacy with elected officials in Washington. Representatives Kevin Hern (R-Okla.) and Terri Sewell (D-Ala.) have introduced a bill in response to the proposed rule. The Home Health Stabilization Act of 2025 would halt home health cuts in 2026 and 2027.
Increased home health aide usage saves Medicare even more money
Home health care is medical care that can be provided by a skilled nurse and physical, occupational, and speech therapists, as well as a home health aide under the supervision of a skilled nurse. For our analysis, we wanted to know how home health aide usage impacts care costs.
What we learned is that increasing the dosage of home health aide support appears to contribute to lower overall expenditures for Medicare, as patients seem to rely on home health aide services more than expensive inpatient, out-patient, ER, and skilled nursing facilities.
And when we looked at beneficiaries with complex, chronic conditions who received a high dosage of home health aide support, we saw that despite their higher acuity, they had in-patient costs that were virtually the same as lower-acuity patients (think: knee replacement) who required only skilled services. And patients receiving high aide support had lower ER and outpatient costs.
High aide users spend less on in-patient, outpatient, and ER care
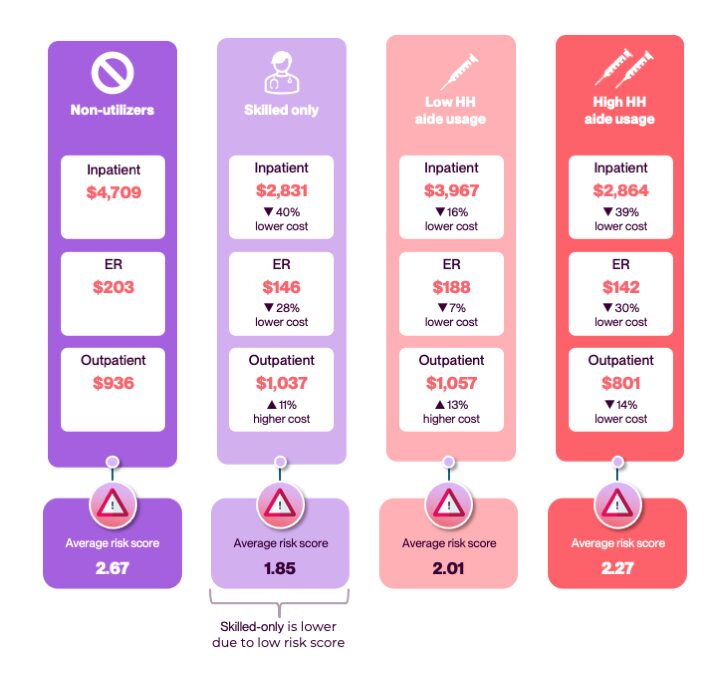
What this suggests is that more readily employing the use of home health aides may help redirect care from institutional settings to the home, contributing to lower overall expenditures.
We’ll all pay the price for reduced access to home health care
Home health providers already face financial pressure at the current payment rates, due to rising operational costs. Further cuts will force more agencies to reduce services, serve fewer patients, or close their doors completely. All while Medicare enrollment is growing exponentially due to our aging population, increasing the demand for this cost-saving care model.
Reduced access to home health care will also require more working tax-payers to reduce their hours or leave their jobs entirely to care for their family members on Medicare. Per the Caregiving in the USA 2025 report recently published by AARP and the National Alliance for Caregiving, 63 million Americans are currently providing care to family members. Every one of them who has to work fewer hours or leave a job to manage care responsibilities contributes less in taxes, social security, and productivity.
Millions of unpaid family caregivers have to live off their own retirement savings to afford to care for an aging family member. This causes many of them to require government assistance, increasing federal spending further.
As our population continues to age, more Americans will be forced to contribute less to our country’s fiscal stability, and instead require more government support.
RubyWell believes that our nation’s aging and disabled citizens deserve to have access to affordable care. We believe that families should not have to bear all of the responsibility for the care of their aging loved ones alone. And we believe that healthcare is a right and not a privilege, no matter who you are or where in the country you live.
But even if one shares none of those beliefs, the very basic math tells us that the U.S. simply cannot afford to reduce access to Medicare’s home health benefit.
Action item: Find contact information for your US representative and senators. Then reach out and ask them to support the Home Health Stabilization Act of 2025.
Because if the goal of CMS is to identify efficiencies and save money in 2026 and beyond, it should enact rules that incentivize more access to home health care and home health aide support, not cut reimbursement for, thereby limiting access to these services. You’re welcome to include an attachment of our report in your correspondence.